 BY Ariel Kelly, Associate, Fisher Phillips
BY Ariel Kelly, Associate, Fisher Phillips
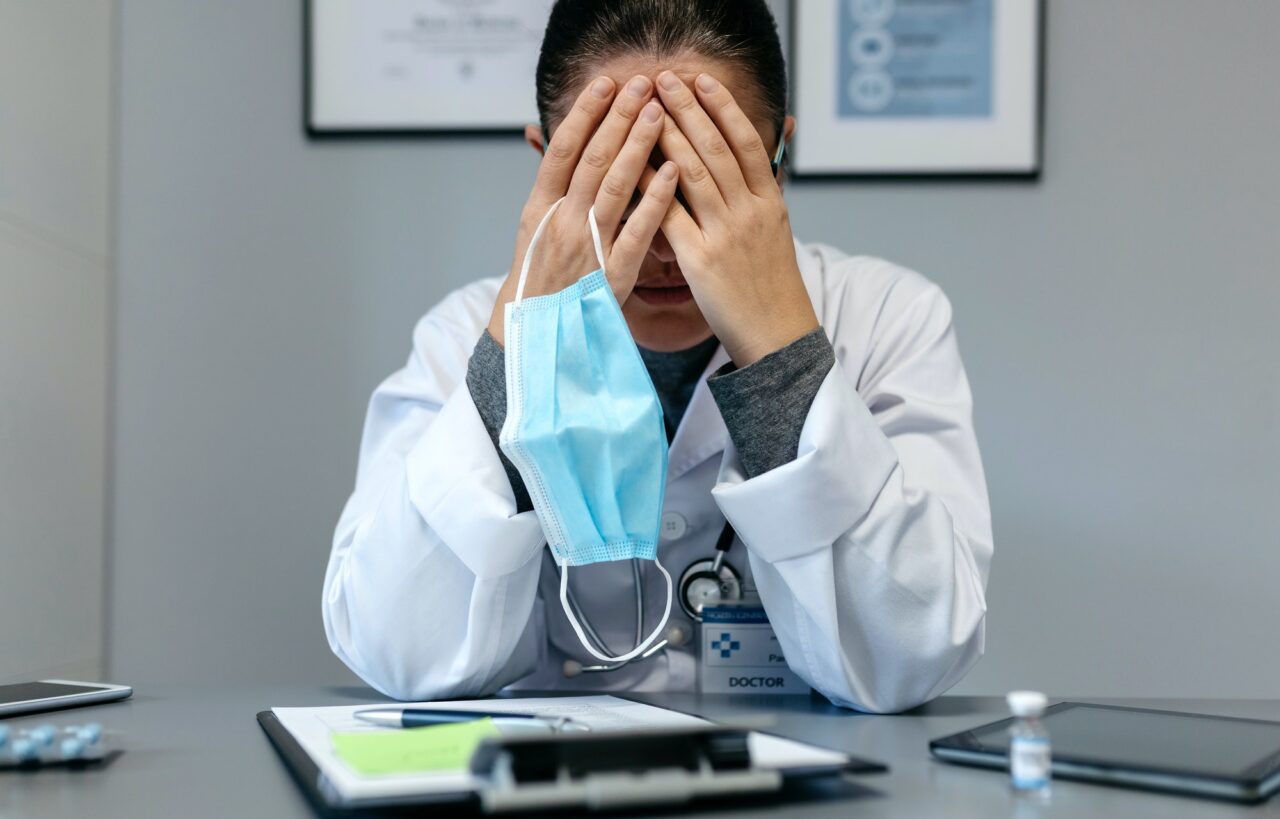
The COVID-19 pandemic continues to highlight both the heroism of and challenges facing frontline healthcare workers. Like the rest of us, these heroes are still human and thus experiencing fatigue. According to the American Medical Association, research studies illustrate that half of the health workers have reported COVID-19 burnout. Also known as “COVID fatigue,” COVID-19 burnout affects everyone differently and takes many forms, including physical fatigue, stress, anxiety, exacerbation of mental health issues, and negative mood disposition. Like other states, COVID fatigue has especially hit the Texas healthcare workforce.
Though possibly more prevalent among frontline workers, organizations are feeling this phenomenon across the board. This includes workers in administrative and allied health roles, all of who have experienced the feeling of burnout from countless COVID-related rules and guidance. Some are overwhelmed by seemingly ever-changing and sometimes conflicting COVID rules. Throughout the pandemic, employers have had to adapt, seeking the best ways to implement COVID rules to protect employees and patients.
On top of these challenges, a healthcare staffing crisis and overall labor shortages also threaten the retention of critical workers. For example, even before the COVID-19 pandemic, in 2019, the Texas Center for Nursing Workforce Studies analyzed nursing workforce trends and concluded that demand for registered nurses was estimated to exceed supply every year from 2018 to 2032. Such labor shortages in Texas were only exacerbated when the COVID-19 pandemic hit and have not recovered. Confined by the shortage, but immediate need, of healthcare workers, due to the continuing COVID-19 pandemic, many Texas healthcare facilities turned to short-term employment arrangements, creating the arrangement more commonly known as “travel nursing.” These short-term employment arrangements were also available to other healthcare workers, such as respiratory therapists. While short-term employment arrangements provide a temporary fix, health care facilities may pay considerably more to healthcare workers on short-term assignments than in permanent roles and will still face the same staffing challenges once the contracted, short-term employment period inevitably ends. So, while short-term employment arrangements are an option, Texas healthcare facilities can create a comprehensive plan to address COVID fatigue and retain their existing workforce.
While there is no universal solution, various public health agencies, medical organizations, and research institutions have studied potential solutions. Specifically, the Centers for Disease Control and Prevention provides a spectrum of practical suggestions to help employers combat COVID fatigue, which may also help with employee retention. One suggestion, which can be tailored to the unique challenges that Texas healthcare employers face, is to institute a targeted fatigue risk management plan.
Because the pandemic has become a marathon of sporadic COVID surges with no definitive end in sight, employers should consider designing their own fatigue risk management plan specific to their workforce and regularly update it to adjust to changing circumstances. The risk management plan would focus on safety among staff and patients, hopefully assisting with the retention of the workforce. Five practical strategies to consider when instituting a COVID fatigue risk management plan are:
- Identify and Assess Risk Factors: Begin by collecting information and data to identify risks and address the needs most important to your workforce. You can collect information informally by closely listening to staff concerns during meetings and around the departments. Or, employers can collect information more formally by establishing regular check-ins with staff, conducting anonymous surveys, or directly posing questions related to COVID fatigue.
- Establish Clear Lines of Communication: No matter how you collect information regarding the effects of COVID fatigue, clear lines of communication are critical to ensure that your information gathering will prove productive. Employers should therefore ensure that leaders are visible, engaged, and prepared to facilitate productive dialogue with employees regarding concerns related to COVID fatigue.
- Demonstrate Responsiveness to Employee Concerns: If there is a common sentiment or complaint, employers should address the major concerns and communicate what they are doing to be responsive. Even minor adjustments or responses, whether it involves scheduling, availability of supplies, or creative compensation options, can be invaluable to building trust and teamwork, showing employees that their leaders are committed to maximizing both their safety and morale.
Even small acknowledgment and appreciation can demonstrate responsiveness to employee feedback. In fact, showing appreciation, either through monetary or non-monetary awards, can help sustain and/or re-ignite motivation when COVID fatigue has set in. Even verbal acknowledgment of employees’ hard work and dedication can help show employees that they are valued.
- Provide Appropriate Resources and Information: While identifying challenges in employees’ minds, you should also remind employees of any existing employee assistance programs (“EAP”) or mental health resources that may help them navigate COVID fatigue. In sharing resources and learning more about employees’ challenges, employers must remain cognizant of legal parameters and any requirements to engage in an interactive accommodation process, if applicable. Further, employers must not allow the use of EAP resources to be viewed negatively in any way. Instead, employees should feel comfortable exploring these options. A reminder of existing EAP programs helps assure employees of your commitment to maintaining a supportive, responsive workplace.
Some Texas health care facilities are already trying this approach. For example, some hospitals have opened emotional wellness clinics for employees and their children and lessened the costs of visits to in-network mental health providers. While time will tell how effective these additional resources are in retaining healthcare workers and preventing COVID fatigue, many facilities have seen an initial, positive response from their employees.
- Regularly Assess Workloads: In this era of staffing shortages, do not forget to monitor and assess workloads constantly and, once again, communicate an overall shared commitment to both patients and your staff. For off-shift workers especially, be visible and responsive. And be sure to permit adequate time between shifts to help employees get the rest they need.
Despite the challenges facing Texas healthcare employers, there are opportunities to address COVID burnout among employees. A successful COVID fatigue risk management plan can help improve dialogue between employees and management to help address the concerns and worries that are most important to those on the front lines.


One comment
Pingback: Nashville Attorney Offers Insight on How Healthcare Employers Can Mitigate COVID-Related Burnout & More Latest News - News
Comments are closed.