By Beth Anne Jackson and Elizabeth Jepson, Brown & Fortunato, P.C.
By Beth Anne Jackson and Elizabeth Jepson, Brown & Fortunato, P.C.
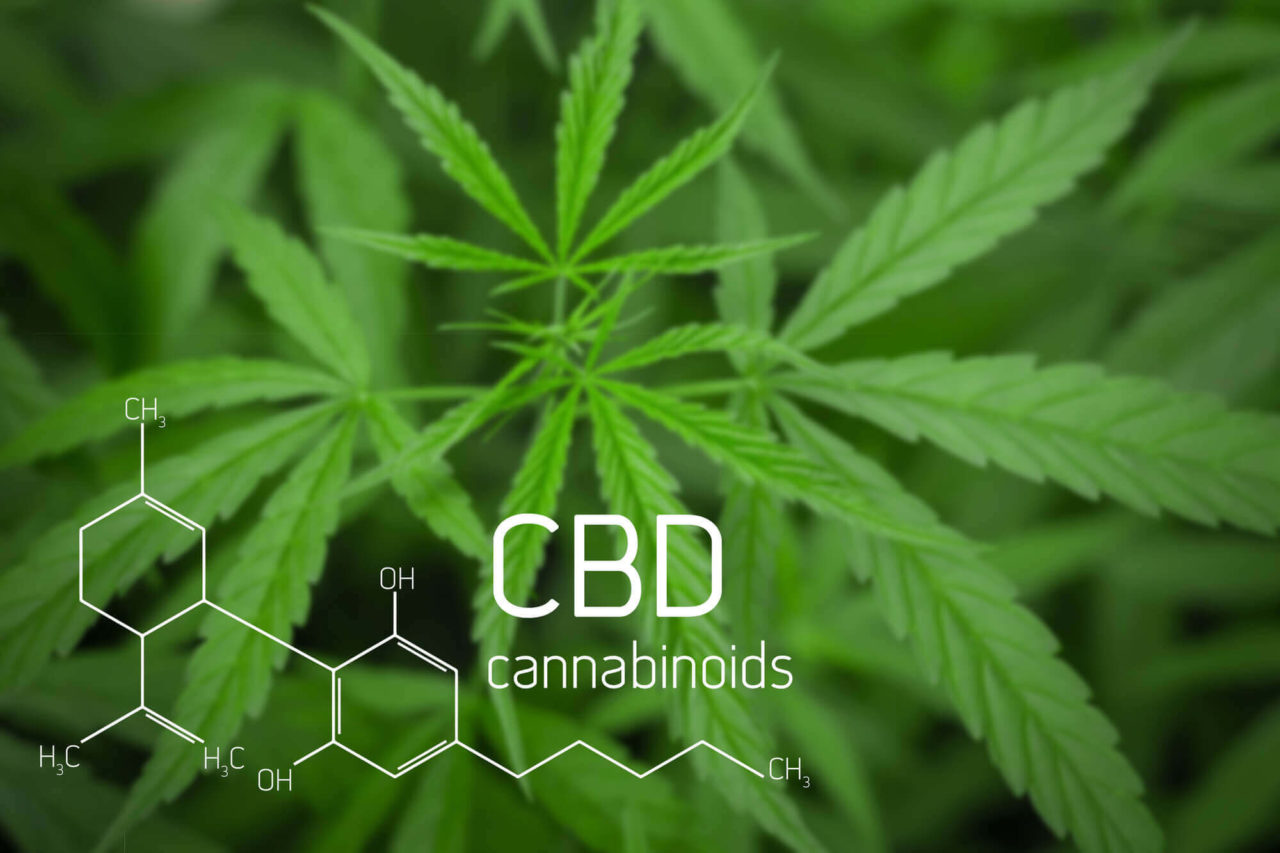
With the passage of the Agriculture Improvement Act of 2018 (Farm Bill) in December 2018, Congress established a new category of cannabis: hemp, which is defined as cannabis with 0.3 percent or less concentration of compound delta-9-tetrahydrocannabinol (THC). Further, the Farm Bill specified that the definition of the term “marihuana” under the Controlled Substance Act does not include “hemp.”
Many assumed that the exclusion of hemp from the definition of marijuana (which is a Schedule I illegal substance) made all cannabidiol (CBD) derived from hemp legal. However, the Farm Bill only legalized products derived from hemp that are produced in accordance with the Farm Bill, which requires the hemp to be produced by licensed growers pursuant to state or federal regulations. Nevertheless, sales and advertising of CBD products, including CBD oils, balms and tinctures, have soared. Many patients may be using CBD and may list it on their medication/supplements list. And some health care providers may be considering, or may already be, selling CBD products.
But physicians should advise and exercise caution for several reasons. First, the legality of products currently on the market is unclear. A statement from departing federal Food and Drug Administration (FDA) Commissioner Scott Gottlieb, M.D. on April 2, 2019, emphasized that the Farm Bill “explicitly preserved the FDA’s current authority to regulate products containing cannabis or cannabis-derived compounds under the Federal Food, Drug and Cosmetic Act (FD&C Act) and section 351 of the Public Health Service Act.” What that means is that CBD derived from hemp produced in accordance with the Farm Bill may be legal, depending on the purpose for which it is sold. It cannot be sold as a dietary supplement or food additive, according to the FDA, because CBD is the active ingredient in the FDA-approved drug Epidiolex®. As such, CBD is statutorily excluded from the definition of “supplement” unless and until the FDA, in its discretion, issues a regulation establishing that the substance is lawful as a supplement. For the same reason, it cannot be added to food. Second, some CBD sellers and manufacturers have made multiple unproven and egregious claims that could lead to patient decisions to forgo clinically proven standard treatments for serious medical conditions. In fact, the FDA has issued warning letters to companies making claims that CBD prevents, treats or cures life-threatening diseases such as cancer, Alzheimer’s disease, and opioid addiction. Patients may fall victim to such claims, and their health care providers may need to inquire further about compliance with prescribed medication regimens if the patient is also using CBD. The final reason for advising caution is that CBD products currently on the market – with the possible exception of products from states that have legalized cannabis – are not regulated and quality control is often poor, meaning that products may not be effective or worse, may be contaminated. Manufacturers may not be following the Current Good Manufacturing Practice regulations for drug products and, consequently, their products may ultimately be deemed “adulterated” or “misbranded” by the FDA.
Health care practitioners whose patients are consuming CBD products face a conundrum: patients may be ingesting products that are not regulated or quality controlled; patients may be taking CBD in lieu of established, proven treatments; and yet, patients may ask their health care provider for advice on using CBD, including dosages and form (e.g., oil or balm). Physicians and other providers should be prepared to advise their patients on the legal status of these products, the fact that they are unregulated, the risks associated with unregulated products, and, if the physician has done sufficient research of the literature, their clinical opinion of CBD products. Certainly, given the number of people using CBD products (estimated at 7% of Americans), every physician should be aware of the effects of CBD use, including but not limited to its impact on biological processes utilizing CYP450 enzymes (e.g., processing of medications such as steroids, calcium channel blockers, HIV antivirals, antibiotics, beta blockers, NSAIDs, antidepressants and others, as well as the metabolization of alcohol).
CBD use will continue to cause clinical and risk management challenges for health care providers. With respect to patient care, being educated about CBD and its uses, risks and potential benefits is quickly becoming the standard of care, and physician are well-advised to incorporate learning about CBD into their continuing education or reading plans. As for selling CBD products, health care providers face legal risk, including potential licensure and DEA action, for doing so, at least until the FDA issues regulations approving CBD as a supplement or food additive. The FDA has scheduled a public hearing for May 31, 2019, regarding CBD products and is accepting written public comments from all stakeholders, including health care providers. The evolving status of CBD products can be followed on the FDA website or contact a qualified attorney for advice.